Spine & Neurosurgeon
Venkateshwar Hospital , Delhi, India23 Years of experience
Speaks: English
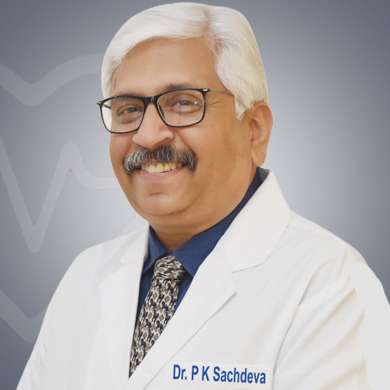
With rich experience of more than 22 years, Dr. P K Sachdeva is a highly acclaimed neurosurgeon in the Delhi-NCR region. He is currently the Director and HOD Neurosurgery at Venkateshwar Hospital, Delhi. Dr. Sachdeva has done his medical graduation in 1989 from Maulana Azad Medical College, New Delhi. In 1995, he did his MS in General Surgery from Lady Hardinge Medical College. He completed his M.Ch. in Neurosurgery from GB Pant Hospital, New Delhi in 1999. Dr. Sachdeva was associated with reputed institutions in India and abroad such as Primus Super Specialty Hospital and Royal Preston Hospital, UK. He was also the Additional Director, Neurosurgery at Fortis Hospital, Shalimar Bagh.
With a Fellowship in Gamma Knife Radio-Surgery from New-York Medical School, USA, and Cyberknife training at Miami Cyber Center, Miami, USA, Dr. Sachdeva is highly experienced in performing the neurosurgical procedures with advanced technology. He performs Spine Surgery, Spinal Fusion Surgery, Deep Brain Stimulation surgery, Brain Tumor Surgery, and Laminectomy with a high success rate. He has a keen interest in various advanced neurosurgical procedures including Spinal Stabilization, Costo-Transversectomy, Spinal Arteriovenous Malformation (AVM) treatment, Lumbar Spondylosis Treatment, Vertebroplasty, Spinal fusion, and Decompression Craniotomy.
Neurosurgeons are trained to treat people suffering aneurysms, blocked arteries, trauma to the brain and spine, birth defects, chronic low-back pain, brain and spinal cord cancer, and peripheral nerve problems. Neurosurgeons also do surgeries for carpal tunnel syndrome, spinal surgery, and brain tumor removal surgery. Here is a list of some of the conditions Dr. P K Sachdeva treats:
Some of the signs and symptoms of neurological disorders are listed below. Consult your doctor/neurosurgeons if you experience any of these symptoms. Early detection of the condition can help control the severity of the symptoms and can be effectively treated. The below symptoms should be discussed with a neurosurgeon who will advise required diagnostic tests and start appropriate treatment.
When the brain is damaged, it affects different things, including memory, sensation, and even an individual’s personality. Brain disorders are caused by illness, genetics, and traumatic injury. These disorders can produce different symptoms.
The working hour of doctor P K Sachdeva is 11 am to 5 pm from Monday to Saturday. The doctor has an off on Sunday. Call the doctor or his attendant to confirm his/her availability because the doctor may not be available due to some personal reasons or any emergencies.
The popular procedures that Dr. P K Sachdeva performs are listed below:
Dr. P K Sachdeva is a renowned neurosurgeon who is known for his patient-centric approach and high success rate. The doctor evaluates the condition of the patient completely before performing any procedure to understand the risk associated with the procedure. With vast experience in performing even the most complex cases with high precision and accuracy, the doctor follows medical protocols in order to ensure patient safety. Also, the doctor is abreast with the latest techniques.

Share Your Experience about Dr. P K Sachdeva

Dr. P K Sachdeva has over 24 years of experience in his field of surgery.
Dr. Sachdeva specializes in performing neurosurgical procedures with advanced technology. He performs Spine Surgery, Spinal Fusion Surgery, Deep Brain Stimulation surgery, Brain Tumor Surgery, and Laminectomy with a high success rate.
Yes, Dr. P K Sachdeva provides online video consultation through MediGence.
It cost 35 USD to video consult with Dr. P K Sachdeva through MediGence.
Dr. Sachdeva is a part of many different medical associations that are internationally and nationally recognized.
Whenever a patient has an ailment of the brain or the related nerves which needs to be surgically corrected such as a patient requiring VP shunt surgery then a Neurosurgeon is the doctor who is best qualified to operate on the patient.
He can be easily consulted by registering your profile with MediGence and writing down your inquiry. A meeting with the surgeon will be scheduled. Following which the consultation can be done.
Dr. P K Sachdeva is a renowned neurosurgeon who is known for his patient-centric approach and high success rate. The doctor evaluates the condition of the patient completely before performing any procedure to understand the risk associated with the procedure. With vast experience in performing even the most complex cases with high precision and accuracy, the doctor follows medical protocols in order to ensure patient safety. Also, the doctor is abreast with the latest techniques. Neurosurgeons work in different settings like private clinics and public or private hospitals. They often collaborate with other specialists and medical professionals as per the requirement of surgery. They also evaluate the condition of the patient before performing surgery in order to find the complications of the surgery, if any.
Diagnosis tests act as an important tool to find out the condition(s) a patient is suffering from. So, a neurosurgeon will ask you to get a few tests done so that they get to know the cause of the symptoms which further helps in finding the condition the patient is suffering from. Based on the diagnosis, the doctor can start appropriate treatment. A neurological exam or a neuro exam is the evaluation of an individual’s nervous system to know how well it is functioning and find out an underlying condition. A neurological exam may include:
The below-listed are some of the diagnostic tests recommended by a neurosurgeon to diagnose a condition of the nervous system::
If you show the below symptoms, consult a neurosurgeon who will diagnose the condition and suggest the right treatment.
Neurosurgeons help in the diagnosis and treatment of the conditions of the nervous system. They are mostly involved in complicated surgery of the brain. They offer surgical treatment for the conditions affecting any part of the body, caused mainly due to nerve issues.